How Long To Wait For Mri After Knee Injury
- Research article
- Open up Access
- Published:
Timing of magnetic resonance imaging affects the accuracy and interobserver agreement of anterolateral ligament tears detection in inductive cruciate ligament scarce knees
Knee Surgery & Related Research volume 32, Article number:64 (2020) Cite this article
Abstruse
Purpose
We aimed to identify the anterolateral ligament (ALL) tears in anterior cruciate ligament (ACL)-deficient knees using standard i.5-Tesla magnetic resonance imaging (MRI).
Methods
Nosotros included all patients who underwent master ACL reconstruction at our center betwixt 2012 and 2015. Exclusion criteria included patients with multiple ligament injuries, lateral collateral ligament, posterolateral corner, and infections, and patients who underwent MRI more than 2 months later their injury. All patients (n = 148) had ACL tears that were afterward arthroscopically reconstructed. The magnetic resonance (MR) images of the injured knees performed within 2 months of injury were reviewed by a musculoskeletal radiologist and an orthopedic surgeon. The patients were divided into two groups. The kickoff grouping of patients had MRI performed within 1 calendar month of injury. The 2nd group of patients had MRI performed i–2 months after the index injury. Both assessors were blinded and the MR mages were read separately to assess the presence of ALL, presence of a tear and the location of the tear. Based on their readings, interobserver understanding (kappa statistic (K)), sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy were compared.
Results
The ALL was identified in 100% of the patients. However, there was a discrepancy of up to xv% in the identification of tear of the ALL. In the first group in which MRI scans were performed within ane month of injury, the ALL tear was identified by the radiologist in 92% of patients and by the surgeon in xc% of patients (Κ = 0.86). In the 2nd group in which MRI scans were performed inside 1–2 months of the injury, the ALL tear was identified by the radiologist in 78% of patients and by the surgeon in 93% of patients (K = 0.62).
Decision
The ALL tin can be accurately identified on MRI, but the presence and location of ALL tear and its location cannot be reliably identified on MRI. The accuracy in identification and label of a tear was affected by the interval between the time of injury and the time when the MRI was performed.
Level of testify
Diagnostic, level IIIb, retrospective.
Introduction
Claes et al. described the presence of the anterolateral ligament (ALL) consistently seen in the lateral side of the knee joint. The ALL was described to be an extra-articular construction with attachment from the lateral femoral condyle to the lateral meniscus and the lateral tibial plateau [1]. Subsequently, biomechanical, cadaveric, and radiological studies were conducted to verify the function and function of the ALL [2,3,iv].
There is a big caste of variation (51–100%) in the sensitivity of magnetic resonance imaging (MRI) for identification of the ALL [5,half dozen,7,8,9]. Macchi et al. and Helito et al. described the visibility of the three segments of the intact ALL in the uninjured knee joint, but did non examine knees with ALL tears [vii, eight].
Other studies accept evaluated agreement between musculoskeletal (MSK) radiologists or between MSK radiologists and orthopedic surgeons, with regards to the ALL, ALL tears, and the location of ALL tears seen on MRI. Each study varied slightly in the methodology and this must exist taken into account. Taneja reported good agreement (kappa (K) = 0.lxx) betwixt ii MSK radiologists in identifying the presence of the ALL as a structure [9]. Kizilgovz reported practiced agreement (K = 0.784–ane) for the visibility of the various parts of the ALL [10].
Kosy reported skilful agreement (K = 0.854) between two MSK radiologists in identifying ALL injuries [11]. Ferretti reported adequately good agreement (M = 0.60–0.75) between two MSK radiologists and i orthopedic surgeon in characterizing whether or not the ALL tear was consummate [12]. Park also reported Grand values of 0.89–0.93 for agreement betwixt ii radiologists in assessing acute anterior cruciate ligament (ACL) injury in the knee [thirteen].
There have been no studies to evaluate how the timing of MRI could bear on accuracy and interobserver agreement in identifying and characterizing ALL tears. The purpose of this report was to evaluate the prevalence of ALL tear in ACL injury according to the timing of MRI and to assess the understanding betwixt an MSK radiologist and an orthopedic surgeon in the identification of ALL tears.
The authors aimed to institute intra-observer and interobserver understanding for identifying and characterizing the ALL and ALL tears in ACL-deficient knees, using standard 1.five-Tesla MRI. The authors hypothesized that interobserver agreement for identification of ALL tears would be high. The authors also hypothesized the interobserver agreement for identification and label of ALL tears would decrease with increase in the duration between index injury and the MRI.
Methods
This was a retrospective study in a cohort of patients with ACL injury. Institutional review lath approval was obtained for this research. Nosotros included all patients who underwent arthroscopic ACL reconstruction with hamstring graft betwixt 2012 and 2015 and who had preoperative MRI performed within 2 months of their injury. Patients with Segond fracture identified on radiographs and MR images were included in this study. We excluded patients with injury to the medial and/or lateral collateral ligament requiring surgical repair or reconstruction, patients with posterolateral corner injury, and patients with concomitant fractures or who underwent combined ligamentous reconstruction. Patients who underwent preoperative MRI more than 2 months afterward their injury were as well excluded.
All MRI was performed at our eye using the Magnetom Aera 1.5-Tesla (T) MRI scanner (Siemens AG, Berlin and Munich). The MRI parameters and the main sequences used for identification of the ALL were centric and coronal proton density-weighted turbo spin echo images (Tabular array 1).
Our patients were stratified into ii groups - ACL-scarce patients who underwent MRI within 1 calendar month of their index injury and ACL-deficient patients who underwent MRI more than i month but within 2 months of their index injury. This stratification was chosen because scar tissue sets in inside 3–4 weeks after injury. Therefore, MR images obtained within a month would demonstrate minimal scarring, and MR images and accuracy may be affected in one case scar tissue develops between 1 and ii months after injury. The authors propose that once scarring sets in, the acutely injured structures would be more difficult to place on MRI.
The MR images were read twice each by a fellowship-trained MSK radiologist and an orthopedic surgeon. They were first asked to identify the ALL according to the protocol described by Helito et al. [7]. If they were able to identify the ALL on MRI, they were then asked to identify if there was a tear in the ALL. If an ALL tear was present, they were asked to identify the location of the tear (i.e. femoral, meniscal, tibial). Figure 1 shows the normal radiological features of the ALL; Fig. ii shows the radiological features of injury to the femoral part of the ALL and Fig. 3 shows radiological features of injuries to the meniscal and tibial parts of the ALL.
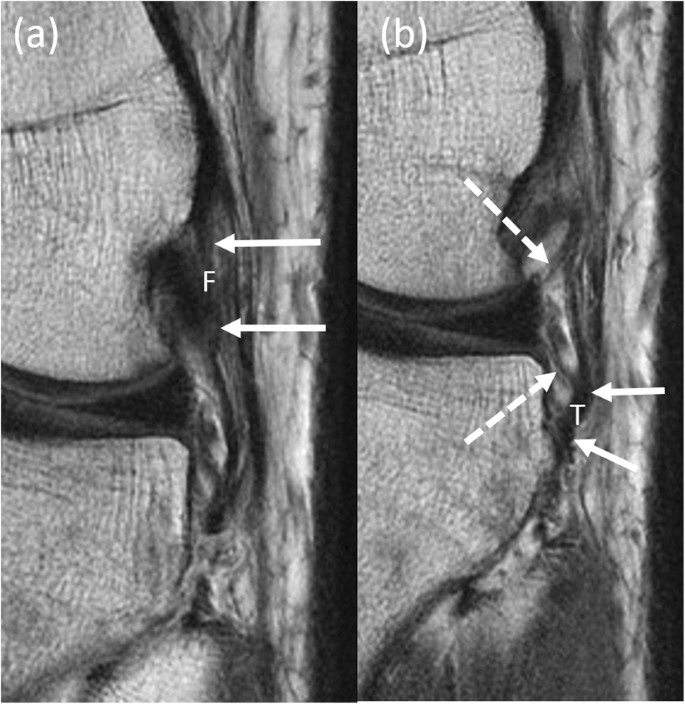
Normal radiological features of the anterolateral ligament (ALL). Serial coronal proton density weighted magnetic resonance (MR) images of the left genu in a 21-year old patient demonstrate the normal features of the femoral (a) (F, solid white arrows) and (b) meniscal (dashed white arrows) and tibial (T, solid white arrows) portions of the ALL
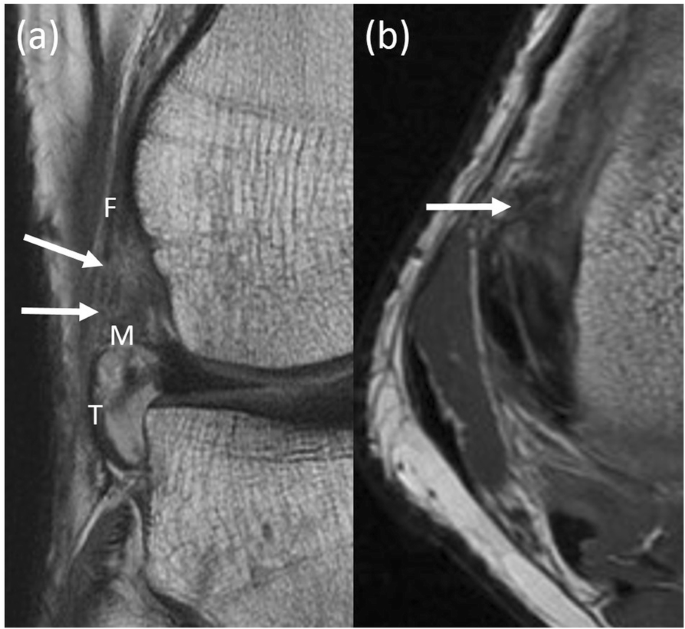
Radiological features of injuries to the femoral part of the anterolateral ligament (ALL). Coronal (a) and axial (b) proton density weighted magnetic resonance (MR) images of the right knee joint in a 32-year former patient demonstrate focal discontinuity, in keeping with a tear of the femoral (F, solid white arrows) portion of the ALL. The intact appearance of the meniscal (One thousand) and tibial (T) portions is also shown
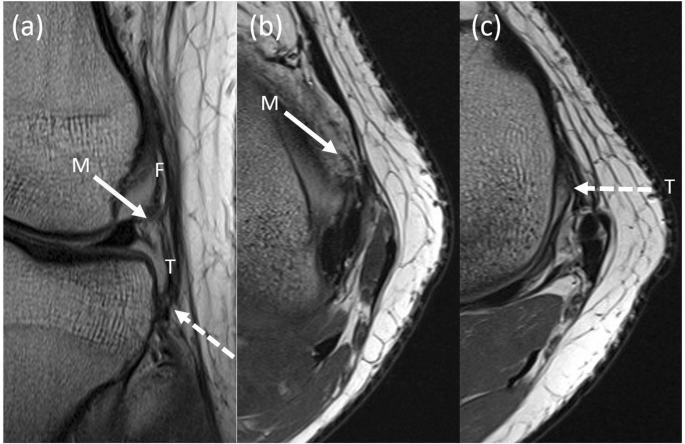
Radiological features of injury to the meniscal and tibial parts of the anterolateral ligament (ALL). Coronal (a) and axial (b and c) proton density magnetic resonance (MR) images of the left knee in a 22-year old patient demonstrate focal irregular attenuation, in keeping with tears of the meniscal (M, solid white arrows) and tibial (T, dashed white arrows) portions of the ALL. The femoral (F) portion is also shown and appears intact
Helito et al. described the ALL based on previous anatomical studies - femoral, meniscal, and tibial. The femoral office of the ALL was defined as the origin to the bifurcation bespeak. The meniscal part of the ALL was defined as the bifurcation indicate to the meniscal insertion. The tibial part of the ALL was defined as the bifurcation to the tibial insertion [7].
The readings made by the MSK radiologist and the orthopedic surgeon were then compared for the calculation of intra-observer and interobserver understanding. In this study, the readings of the MSK radiologist were taken as the gold standard in view of his more all-encompassing experience in MSK imaging. The accuracy of the orthopedic surgeon in determining if there was an ALL tear and the location of the tear on the MRI was referenced confronting the findings of the MSK radiologist.
Statistical analysis
All statistical assay was performed using IBM SPSS Statistics 21.0. The observed proportionate understanding and Cohen'due south kappa coefficient were calculated to appraise interobserver understanding in identifying and characterizing ALL tears in patients with ACL-scarce knees. The specificity, sensitivity, positive predictive value, and negative predictive values were also calculated to assess the accuracy of identifying and characterizing ALL tears. Accuracy is divers every bit the number of accurate assessments (true positives + truthful positives) over the number of total assessments (true positives + true negatives + fake positives + false negatives).
Results
Betwixt 2012 and 2015, there were 368 ACL reconstructions performed at our institution. Of these, 220 were excluded because the patients had concomitant posterolateral corner injuries (n = 8) or did not undergo MRI inside ii months of their injury (north = 215). The remaining 148 patients all underwent MRI within ii months of their injury. At that place were 3 patients who brutal into both of these groups.
The patients were divided into 2 groups - group one: patients who underwent MRI within a calendar month of their injury (n = 88) and grouping 2: patients who underwent MRI more than a month merely within 2 months of their alphabetize injury (n = lx).
Identification of the ALL
The ALL was identified on the MRI images in all patients beyond the two groups. There was no intra-observer variation in the readings.
Identification of tears in the ALL
In group 1 (n = 88), the radiologist identified a tear in the ALL in 81 patients (92%) and the orthopedic surgeon identified a tear in 79 patients (90%) (Tabular array ii). The Cohen's K coefficient was 0.86 for identification of ALL tears on MRI performed inside 1 calendar month of the index injury. In group 2 (n = 60), the radiologist identified a tear in the ALL in 47 patients (78%) and the orthopedic surgeon identified a tear in l patients (83%). The two assessors were in agreement on the assessment of 37 of the patients. The Cohen's M coefficient was 0.62 for this group. The identification of a tear of the ALL was between two and ix% discrepant depending on the interval of time between the MRI and the injury. Non identification of the presence of a tear on MRI was affected by the fourth dimension interval between the injury and the conquering of MRI (p value <0.01).
The sensitivity for identification of ALL tears was 0.91 in grouping 1 and 0.79 in grouping 2. The positive predictive value for patients in grouping one was 0.94, whereas it was 0.74 for patients in group 2. The negative predictive value for identification of ALL tears in group 1 was 0.22. Accuracy for identification of ALL tears reduced over time; the accuracy in group 1 was 0.86, but was only 0.62 in group ii.
As observed in Table 2, there was a trend toward lower sensitivity, positive predictive value, negative predictive value, accurateness, and the K coefficient for interobserver understanding, with increasing time interval between the alphabetize injury and the acquisition of MRI. Effigy 4 shows a comparison of the radiological features of ALL injury in group ane and group 2.
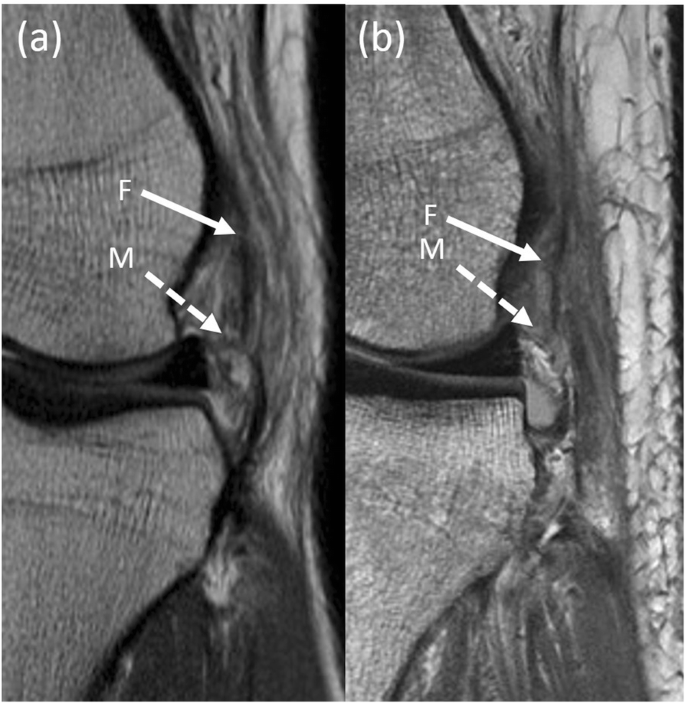
Comparing of the radiological features of anterolateral ligament (ALL) injury in group one and grouping two. Coronal proton density magnetic resonance (MR) images of the left knee obtained less than 1 month afterward injury in a 22-year erstwhile patient (a) and obtained between one and 2 months afterward injury in a 31-yr old patient (b). Focal tear of the femoral portion of the anterolateral ligament (F, solid white arrow) is less conspicuous in (b) as compared to (a), presumably due to scarring which has occurred by the time of imaging. Visibility of the torn meniscal portion of the anterolateral ligament (One thousand, dashed white arrows) is also reduced in (b) equally compared to (a) secondary to background scarring
Identifying location of the tears within the ALL
Afterward being able to identify a tear in the ALL, the radiologist and the orthopedic surgeon were tasked to identify the location of the tear (femoral, meniscal, tibial portion of the ALL). In group 1, threescore femoral-side tears were identified by the radiologist and 41 were identified past the orthopedic surgeon (Table 3). The two readers were in agreement on 43 out of the 88 patients; the K coefficient was 0.09 and the accuracy was 0.54. The radiologist identified 67 meniscal-side tears and the orthopedic surgeon identified 63 of these. The two readers were in agreement on 64 out of 88 patients; the K coefficient was 0.xxx and the accuracy was 0.73. The radiologist identified 19 tibial-side tears and the orthopedic surgeon identified 17 of these. The two readers were in agreement on 70 out of 88 of these patients; the K coefficient was 0.38 and the accurateness was 0.80.
In group 2, the radiologist identified 38 femoral-side tears and the orthopedic surgeon identified 43 of these. They were in agreement on 33 out of threescore patients; the K coefficient for identifying femoral-side tears in the ALL on MRI between i and two months of index injury was − 0.02 and the accuracy was 0.55. The radiologist identified 28 meniscal-side tears and the orthopedic surgeon identified 52 of these. The two readers were in understanding on 32 out of threescore patients; the K coefficient was 0.xi and the accuracy was 0.53. The radiologist identified 3 tibial-side tears and the orthopedic surgeon identified 28 of these. The two readers were in agreement on 35 out of threescore patients; the observed proportionate understanding was 0.58 and the Chiliad coefficient was 0.12.
As observed in Tabular array 3, the interobserver agreement (K coefficient) for identification of location of the tears of the ALL reduced with increasing time interval between the patient's injury and the acquisition of MRI. The other parameters such as positive predictive value, negative predictive value, and accurateness were also noted to reduce with time, only only in the meniscal and tibial groups.
Discussion
Based on our findings, the ALL was identified as a structure in 100% of patients with ACL-scarce knees both past the MSK radiologist and by the orthopedic surgeon. The incidence of ALL tears identified in our ACL-deficient cohort was 90% in patients who underwent MRI inside 1 month of injury. The identification of ALL injuries in ACL-scarce knees was inversely proportional to the time interval between the index injury and the conquering of MRI. Distal ALL (meniscal and tibial) injuries were more than common and were identified with ameliorate accuracy and interobserver agreement as compared to proximal ALL injuries.
The available literature indicates variability in the visualization of the ALL on MRI. Claes was able to place the ALL in 76% of his study accomplice. Other authors report agreement between two radiologists for identification of the ALL every bit a structure in 93–100% of cases [6,seven,viii]. However, Taneja et al. identified the ALL in only 51% of their cohort [nine]. In our report, the ALL was identified both by the orthopedic surgeon and by the radiologist in 100% of patients. Kizilgoz et al. identified the ALL on 82% of 206 MRI examinations performed in patients with knee injuries; 53.3% of their cohort had both ACL and concomitant ALL injury [x]. The incidence of concomitant ALL injuries was xc% in our cohort of patients with ACL-deficient knees.
The K coefficient (g = − 0.02 to 0.38) was low for the identification of tears in various parts of the ALL in our report. This is consequent with the kappa values reported past Hartigan et al. [half dozen]. This suggests that despite being able to successfully identify the various parts of the ALL on MRI, it may not be easy to reliably place the location of ALL tears. Claes reports that 77.8% of ALL injuries occur in the distal tibial portion [5]. Claes divided the ALL into proximal and distal portions. Proximal refers to the part of the ALL from the femoral lateral epicondyle to the meniscofemoral portion and distal refers to the part of the ALL from the meniscofemoral portion to the distal tibial insertion posterior to Gerdy's tubercle [one]. In our written report, the tears on the distal portion (meniscal and tibial tear) represented 68% of the full ALL injuries in group 1, which is like to the Claes study.
Hartigan et al. written report that agreement is poorest in identifying femoral-side ALL tears (chiliad = 0.04–0.14) and tibial-side ALL tears (m = 0.31–0.55) [6]. Similarly, we also noted lower interobserver agreement or kappa values in identifying femoral-side tears (k = − 0.02 - 0.09) equally compared to tibial-side tears (k = 0.12–0.38).
Other authors accept reported better interobserver agreement in their studies. Taneja et al. and Bilfeld et al. conducted studies with a smaller sample size and assessed the understanding between ii MSK radiologists [9, 14]. Ferretti et al. written report better understanding (g = 0.60–0.75) among three readers - two radiologists and ane orthopedic surgeon; however, they identified ALL injuries in a 26-patient cohort based on images acquired using a three T MRI auto [12].
In our written report, it is of import to take into account that nosotros were trying to identify tears in three parts of the ALL in ACL-injured knees. Nosotros study the best interobserver agreement in identifying tibial-side tears of the ALL. This is consistent with the Macchi and the Helito studies where the best identification rates were for tears in the tibial role of the ALL [vii, 8].
Porrino et al. conducted an MRI written report of 53 knees and concluded that details of the ALL were difficult to discern due to the confluence of the ALL with the fibular collateral ligament at its femoral insertion. This could possibly explain the poor understanding in picking upwards femoral-side ALL tears [15]. Another challenge to accurately identifying ALL tibial-side injuries on MRI would be the difficulty in differentiating peripheral tears of the lateral meniscus with injury to the meniscal portion of the ALL.
Devitt et al. performed an MRI report comparing the visibility of the ALL in ACL-injured and ACL-intact knees [xvi]. The visibility of the ALL in three regions - femoral, meniscal, and tibial - was assessed by an MSK radiologist and an orthopedic surgeon. They reported 93% understanding and one thousand = 0.86 for visualization of the ALL in ACL-intact knees, and 71% agreement and thou = 0.52 in ACL-deficient knees. The ALL was identified more reliably in the ACL-intact knees than in the ACL-deficient knees. They reported that the visibility of the ALL was poorest at the femoral side and best at the tibial side, which is like to our findings [sixteen].
Devitt et al. acknowledged that they did not take into consideration the understanding for identifying such injuries in relation to the timing of the MRI [xvi]. In our written report, we looked at the incidence and location of the ALL injury on MRI in a cohort of patients with ACL injury, taking into account the timing of the MRI. Nosotros stratified our results based on the time interval betwixt the index injury and the acquisition of MRI. The length of this interval affected the interobserver agreement for identifying ALL tears. The discrepancy in identifying tears in the ALL when the MRI was performed within ane month of the index injury was 2%. In the other group in whom MRI was performed later on ane month but within 2 months of the index injury, the discrepancy increased to 15% (the MSK radiologist reported ALL tears in 78% of patients, whereas the orthopedic surgeon reported ALL tears in 93% of patients). Therefore, we showed that the longer interval betwixt the index injury and the MRI led to statistically significantly poorer accuracy/interobserver agreement for identification of ALL injuries.
Based on the guidelines proposed by Landis and Koch in 1977, the magnitude of reliability is described as follows: kappa values betwixt 0 and 0.20 indicate slight understanding, values between 0.21 and 0.twoscore bespeak off-white agreement, values between 0.41 and 0.60 bespeak moderate agreement, values betwixt 0.61 and 0.eighty indicate substantial understanding and values betwixt 0.81 and 1.00 betoken well-nigh perfect agreement. A negative value indicates poor understanding [17].
In our report, in that location "almost perfect" understanding between our two assessors in terms of localization of meniscal and tibial-sided tears in group one. However, the understanding was only "substantial" in group ii, farther affirming our previous indicate that the interval between the alphabetize injury and the MRI affects the agreement for identification of ALL tears in every location. It appears that the longer the interval between the index injury and the acquisition of MRI, the more disagreement there is between readers. This could be due to increased MRI scar artefact.
The strengths of our report are the following: (1) all MRI examinations in our report were performed using the same standard sequence using the i.five Tesla MRI machine at our center; (ii) all MR images were read by two specialists (an MSK radiologist and an orthopedic surgeon); (3) we stratified our cohort based on the fourth dimension interval between the index injury and the conquering of MRI; and (4) nosotros studies a larger sample of patients than most of the other studies published on this topic.
Ane limitation that nosotros admit is the utilise of a 1.5-T MRI machine and the 3-mm thickness of the MRI slices. Ferretti et al. report that the rate of failure to characterize the ALL is twice as loftier in patients who undergo 1.5-T MRI compared with iii-T MRI [18]. Patel et al. recommend a 3.0-T MRI system with a dedicated knee coil to achieve a piece thickness betwixt 0.5 and 1.0 mm, to improve define the ALL on MRI [xix]. This indicates that current imaging modalities and protocols may not be sufficiently sensitive to accurately option up ALL injuries. Still, in this study, we used the MRI machines and protocols that we work with. We wanted to determine the ability of surgeons using current imaging modalities to place ALL injuries.
Some other limitation of our study was that later on stratification the tear based on its sub-position on the ALL, the sample size became besides pocket-sized to determine statistical significance when comparison against preoperative knee event scores. Our data on ALL tears and the location of ALL tears also does not assistance us understand which tears are significant, which tears will heal, and nigh importantly, which tears to accost surgically. Further studies will exist required to address all these aspects to decide the best management of ALL injuries in the ACL-deficient knee. However, this study is a step toward understanding the imaging of the ALL. With information technology and with the agreement of the limitations of using MRI to diagnose ALL tears, surgeons can study these tears more closely and then choose to effect their treatment algorithm.
Decision
The ALL can be accurately identified on MRI. The incidence of ALL tears as identified on MRI in a cohort of patients with ACL-deficient knees was loftier at 90%. Distal injuries of the ALL are more than mutual. The time interval betwixt the index injury and MRI is inversely proportional to the accurateness and interobserver agreement for identification of ALL injuries.
Availability of data and materials
Non applicable.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ALL:
-
Anterolateral ligament
- MRI:
-
Magnetic resonance imaging
- MSK:
-
Musculoskeletal
References
-
Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J. Anatomy of the anterolateral ligament of the articulatio genus. J Anat 2013;223(four):321-viii.
-
Caterine S, Litchfield R, Johnson M, Chronik B, Getgood A. A cadaveric study of the anterolateral ligament: re-introducing the lateral capsular ligament. Articulatio genus Surg, Sports Traumatol, Arthrosc 2015;23(11):3186-95.
-
Dodds AL, Halewood C, Gupte CM, Williams A, Amis AA. The anterolateral ligament: anatomy, length changes and association with the segond fracture. Bone Joint J 2014;96-B(3):325-31.
-
Vincent JP, Magnussen RA, Gezmez F, Uguen A, Jacobi Thou, Weppe F et al. The anterolateral ligament of the human knee: an anatomic and histologic study. Human knee Surg, Sports Traumatol, Arthrosc 2012;20(1):147-52.
-
Claes S, Bartholomeeusen S, Bellemans J. Loftier prevalence of anterolateral ligament abnormalities in magnetic resonance images of inductive cruciate ligament-injured knees. Acta Orthop Belgica 2014;80(1):45-ix.
-
Hartigan DE, Carroll KW, Kosarek FJ, Piasecki DP, Fleischli JF, D'Alessandro DF. Visibility of anterolateral ligament tears in anterior cruciate ligament–deficient knees with standard 1.5-Tesla magnetic resonance imaging. Arthrosc. J Arthroscopic Relat Surg 2016;32(10):2061-5.
-
Helito CP, PVP H, Costa HP, Bordalo-Rodrigues M, Pecora JR, Camanho GL et al. MRI evaluation of the anterolateral ligament of the knee: assessment in routine 1.five-T scans. Skelet Radiol 2014;43(x):1421-7.
-
Macchi V, Porzionato A, Morra A, Stecco C, Tortorella C, Menegolo M et al. The anterolateral ligament of the knee joint: a radiologic and histotopographic report. Surg Radiol Anat 2016;38(three):341-viii.
-
Taneja AK, Miranda FC, Braga CAP, Gill CM, LGC H, DCB S et al. MRI features of the anterolateral ligament of the genu, Skelet Radiol 2015;44(3):403-10.
-
Kızılgöz V, Sivrioğlu AK, Aydın H, Çetin T, Ulusoy GR. Assessment of the anterolateral ligament of the knee by 1.5 T magnetic resonance imaging. J Int Med Res 2018;46(iv):1486-95.
-
Kosy JD, Mandalia 6, Anaspure R. Label of the beefcake of the anterolateral ligament of the knee joint using magnetic resonance imaging. Skelet Radiol 2015;44(xi):1647-53.
-
Monaco E, Helito CP, Redler A, Argento Grand, De Carli A, Saithna A et al. Correlation betwixt magnetic resonance imaging and surgical exploration of the anterolateral structures of the acute inductive cruciate ligament–injured knee. Am J Sports Med 2019;47(5):1186-93.
-
Park YB, Lee HJ, Ro DH, Lee GY, Kim South, Kim SH. Anterolateral ligament injury has a synergic impact on the anterolateral rotatory laxity in astute anterior cruciate ligament-injured knees. Knee Surg, Sports Traumatol, Arthrosc 2019;27(x):3334-44.
-
Faruch Bilfeld Yard, Cavaignac E, Wytrykowski M, Constans O, Lapègue F, Chiavassa Gandois H et al. Anterolateral ligament injuries in knees with an inductive cruciate ligament tear: contribution of ultrasonography and MRI. Eur Radiol 2018;28(1):58-65.
-
Porrino J, Maloney E, Richardson Chiliad, Mulcahy H, Ha A, Chew FS. The anterolateral ligament of the articulatio genus: MRI appearance, association with the segond fracture, and historical perspective. Am J Roentgenol 2015;204(2):367-73.
-
Devitt BM, O'Sullivan R, Feller JA, Lash Northward, Porter TJ, Webster KE et al. MRI is not reliable in diagnosing of concomitant anterolateral ligament and anterior cruciate ligament injuries of the human knee. Knee Surg, Sports Traumatol, Arthrosc 2017; 25(iv):1345-51.
-
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33(1):159-74.
-
Monaco Due east, Sonnery-Cottet B, Daggett M, Saithna A, Helito CP, Ferretti A. Elimination of the pin-shift sign afterwards repair of an occult anterolateral ligament injury in an ACL-scarce knee. Orthop J Sports Med 2017;eighteen;5(ix):2325967117728877.
-
Patel KA, Chhabra A, Goodwin JA, Hartigan DE. Identification of the anterolateral ligament on magnetic resonance imaging. Arthrosc Tech 2017 ;30;6(1):e137-e141.
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
Tan Tien Jin, Dave Lee and Tiep Nguyen contributed to reviewing the MR images for the purpose of this report. Audrey Han, Dave Lee, Tiep Nguyen and Tan Tien Jin contributed to assay of the data and manuscript writing. All authors read and canonical the last manuscript.
Corresponding author
Ethics declarations
Ideals approval
This commodity does not comprise whatsoever studies with human participants or animals performed past any of the authors.
Consent for publication
Informed consent was obtained from all individual participants included in the report.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open up Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, accommodation, distribution and reproduction in whatever medium or format, as long as you give appropriate credit to the original author(south) and the source, provide a link to the Creative Commons licence, and betoken if changes were made. The images or other tertiary party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Eatables licence and your intended utilize is not permitted by statutory regulation or exceeds the permitted use, you volition need to obtain permission straight from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Artistic Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/goose egg/ane.0/) applies to the data made available in this commodity, unless otherwise stated in a credit line to the information.
Reprints and Permissions
About this commodity
Cite this article
Han, A., Tan, T., Nguyen, T. et al. Timing of magnetic resonance imaging affects the accuracy and interobserver understanding of anterolateral ligament tears detection in anterior cruciate ligament scarce knees. Articulatio genus Surg & Relat Res 32, 64 (2020). https://doi.org/x.1186/s43019-020-00082-z
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s43019-020-00082-z
Keywords
- ALL, Anterolateral ligament
- ACL, Anterior cruciate ligament
- ACL-deficient, Anterior cruciate ligament deficient
- Radiological
- MRI
- Tear
- Visibility
- Segond fracture
- Diagnostic imaging
Source: https://kneesurgrelatres.biomedcentral.com/articles/10.1186/s43019-020-00082-z

0 Response to "How Long To Wait For Mri After Knee Injury"
Post a Comment